Five Ways to Reduce Diagnostic Error and Malpractice Claims in Clinics
Failure to diagnose atrial fibrillation results in disabling stroke
A 69-year-old man with a history of Parkinson’s disease, stroke and hypertension presented to his neurologist with complaints of lightheadedness. The physician examined the man, noted an irregular heart rate and ordered an EKG. The neurologist documented that if the EKG was abnormal, he planned to refer the man to a cardiologist.
One week later, the neurology clinic received the EKG report, which showed the man had atrial fibrillation. The neurology nurse received the report electronically and was supposed to assign it to the neurologist’s inbox for review. For unknown reasons, the nurse did not send the abnormal EKG report to the neurologist’s inbox, and the neurologist did not order follow-up care.

Five months later, the man presented to his local hospital’s emergency department (ED) with complaints of right facial droop, slurred speech and right-sided weakness. The ED physician diagnosed atrial fibrillation and a large stroke involving the cerebral artery. Following hospitalization, his physician discharged him to a rehab facility. The man later returned home but was disabled by the stroke.
The man and his family filed a malpractice claim against the neurologist and the clinic, alleging failure to timely diagnose and treat atrial fibrillation, resulting in a disabling stroke. The experts who reviewed the care were critical of the clinic for failing to have a reliable follow-up system to review critical test results and communicate results to patients so they can receive prompt treatment. The case was closed with a payment to the man on behalf of the neurologist and the clinic.
Diagnostic error is the top malpractice allegation in clinics
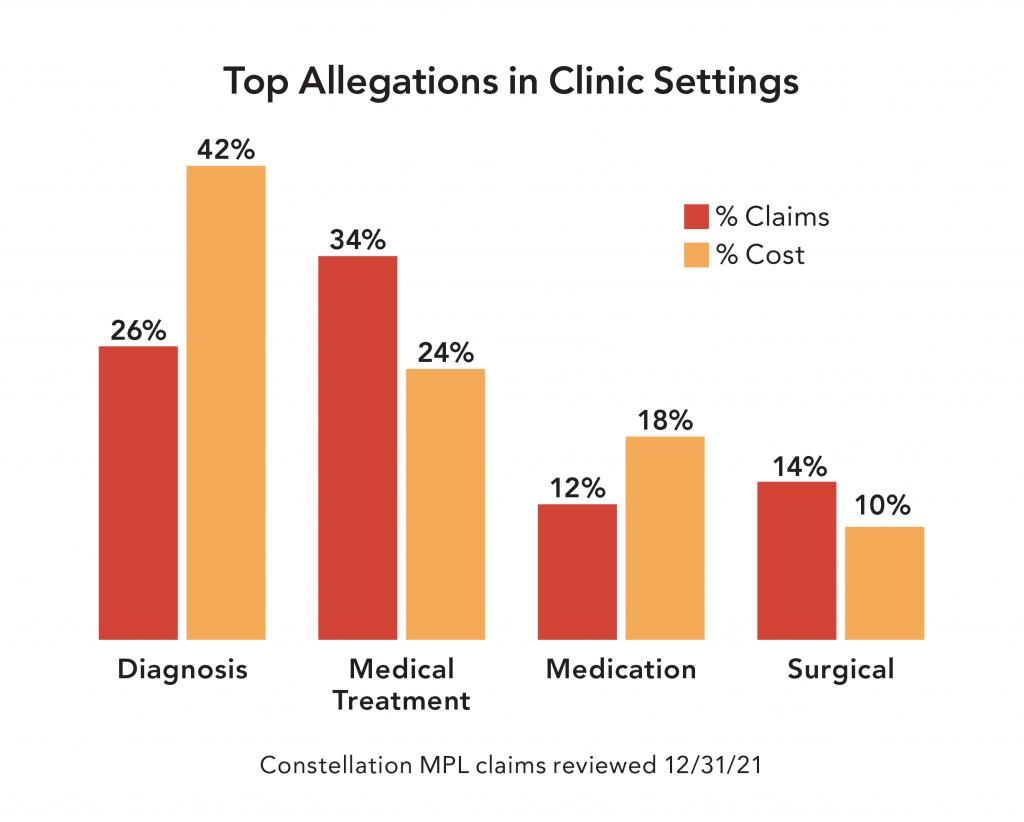
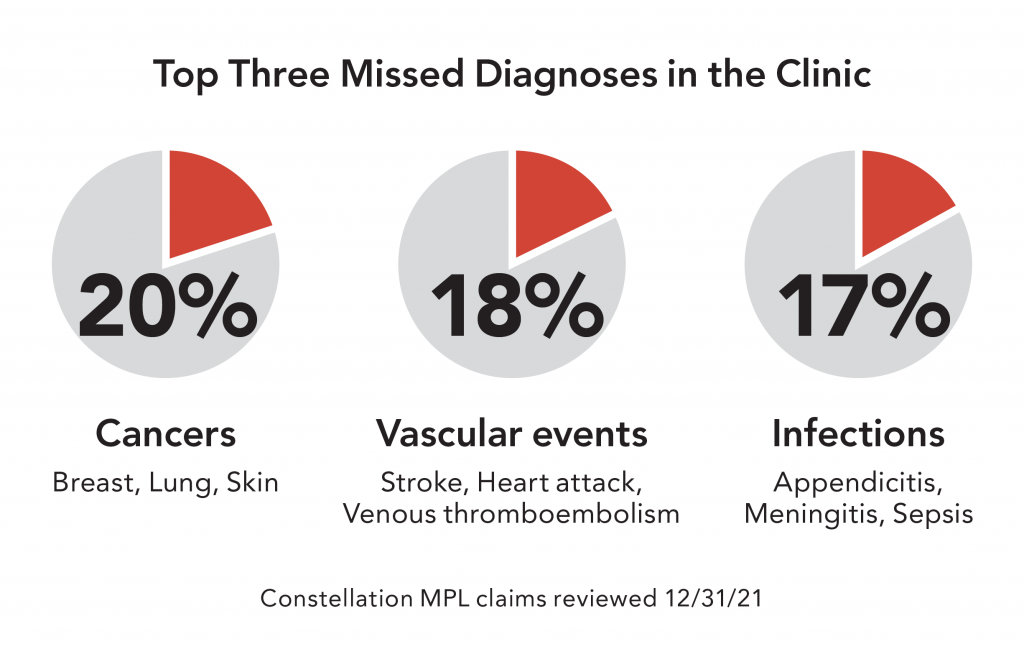
In our analysis of Constellation malpractice claims, diagnostic (Dx) error is the #1 most costly and #2 most frequent allegation. Dx error claims are the most expensive claims for clinics, contributing to almost half of costs (42%), largely due to the severity of harm caused by missed or delayed diagnosis.
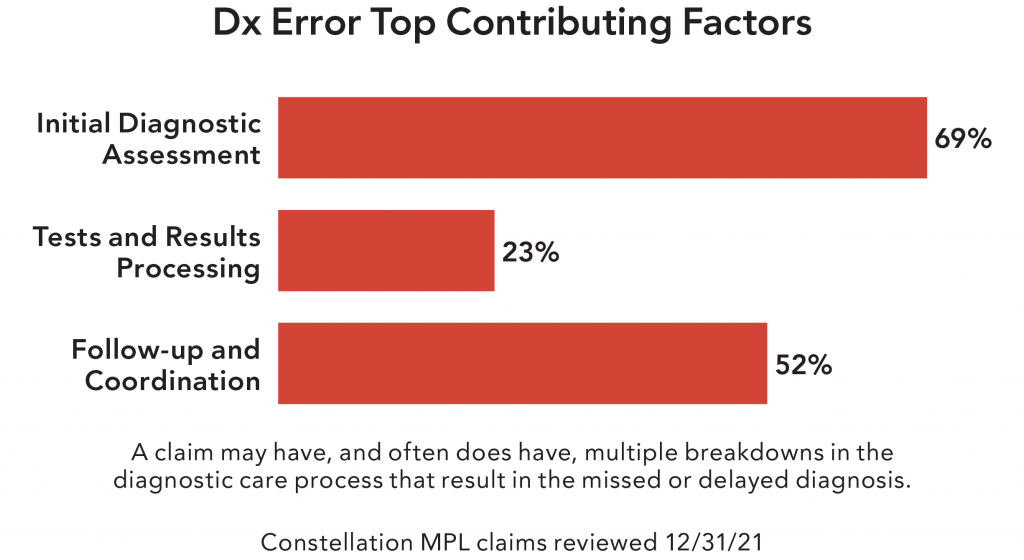
Top contributing factors to diagnostic error harm events in clinics
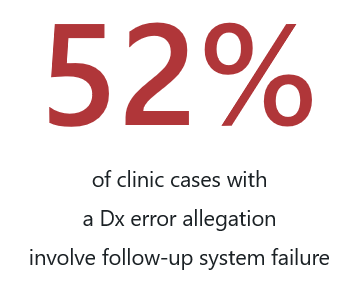
Contributing factors are the risk management issues that contribute to a harm event (or malpractice claim) and are amenable to risk mitigation strategies. Most harm events involve multiple contributing factors. Over half of clinic Dx error cases involve issues with follow-up care and coordination; we call these “follow-up system failures.” The follow-up and coordination stage of the diagnostic care process includes the clinician following up with a patient regarding tests results, referrals to specialists, patient information communicated with the specialist, and the clinician establishing a follow-up care plan with the patient.
View the on-demand webinar: Reduce Follow-Up System Failures and Diagnostic Error With Improved Processes. Constellation and the Society to Improve Diagnosis in Medicine (SIDM) discuss methods clinics can use to identify the return on investment (ROI) on process improvement, find data sources and improve diagnostic processes.
Five ways to reduce diagnostic error in clinics
- Provide clinical decision support tools (e.g., clinical algorithms, artificial intelligence) to help clinicians develop robust differential diagnosis lists and rule out potentially serious conditions.
- Evaluate your follow-up systems to manage diagnostic tests and referrals using a failure mode and effects analysis tool.
- Educate and engage patients to be part of the diagnostic team with statements such as, “If you don’t hear from us about your test results, please give us a call.”
- Implement test management, referral management and critical test management policies outlining highly-reliable processes, systems and communication methods.
- Analyze diagnostic harm events using a root cause/common cause analysis tool and implement strategies to mitigate harm.
Risk reports
Our risk reports analyze Constellation’s malpractice claim data on a wide range of topics and specialties, and share insights clinicians, care teams, clinics, hospitals and senior living organizations can use to help reduce harm events and malpractice claims.
Are you a Constellation client? Sign in to MyAccount to access exclusive customer versions of our risk reports. The expanded reports share actionable insights and strategies that you can utilize to help reduce harm events and malpractice claims. After you sign in, follow Risk Resources > Tools & Resources > Publications > Risk Reports. You also have access to a host of Bundled Solutions (in Risk Resources) that cover a wide variety of topics—such as Preventing Diagnostic Error—to assist you in your risk mitigation efforts.
To learn more about the top drivers of risk in clinics, read our Fall 2022 issue of Common Factors.
Constellation® and Common Factors® are trademarks of Constellation, Inc.
Share this blog article:
Latest Blog Articles
Five Steps to Reduce Generative AI Risks in Healthcare
AI is already assisting physicians and healthcare organizations in many ways. Learn how its use may impact liability and what strategies can mitigate risk.
Five Steps to Reduce Obstetrical Errors and Malpractice Claims
Learn how to reduce obstetrical harm using evidence-based protocols for managing high-risk situations, joint team fetal monitoring education, and enhanced teamwork.
How to Reduce Surgical Harm and Malpractice Claims
In an analysis of our medical professional liability claims, surgical allegations are #1 in occurrence and #2 in cost. Learn how to reduce surgical malpractice risk.
